
Many people know someone who has had a knee or hip replacement. These procedures are common and well-known. Far fewer people know someone who has had their elbow replaced.
That’s because elbow arthritis occurs much less frequently than knee or hip arthritis. As a result, elbow replacements are far less common—and recently, they have become even more rare.
In the past, patients with rheumatoid arthritis were the main group needing elbow replacements. However, newer medications for rheumatoid arthritis have been highly effective at controlling the disease before it causes severe joint destruction. Thanks to these medical advances, the need for elbow replacement surgery in rheumatoid patients has declined.
That said, elbow replacement is still sometimes necessary for patients with severe arthritis, complex fractures, or other conditions that severely damage the joint. But because the surgery is performed less frequently than other joint replacements, finding a surgeon with experience in elbow replacement can be a challenge. This is an important consideration if you’re exploring this option.
As an orthopedic surgeon with a special focus on shoulder and elbow care, I’ve performed elbow replacements for patients in specific situations. Here are the key facts—and misconceptions—you should know if you’re considering this procedure.
Why Elbow Replacements Come With Unique Risks
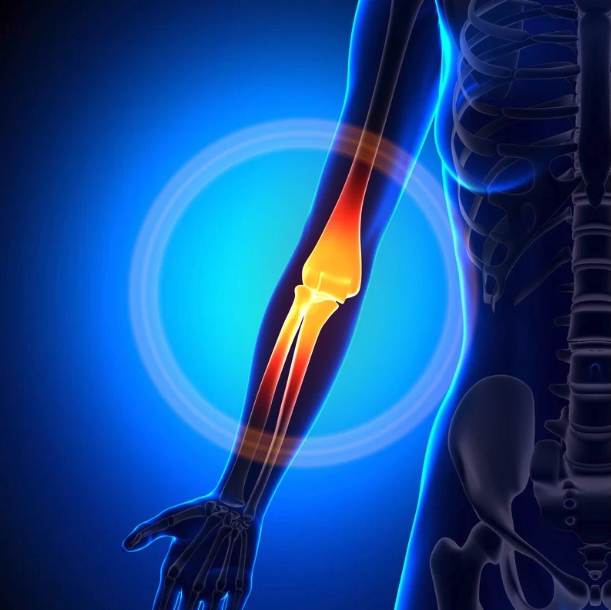
Take a moment to straighten your arm and pinch the skin over the back of your elbow. Now bend your elbow and feel how little soft tissue lies between your skin and the underlying bone. Unlike the hip or knee, which are well-protected by layers of muscle and soft tissue, the elbow has only a thin covering of skin and subcutaneous tissue.
This limited soft tissue means the elbow is at a higher risk for wound healing complications after surgery. The thin skin and lack of protective muscle around the joint make postoperative infections, wound breakdown, and skin irritation more likely.
Because of this, surgeons take special precautions during and after elbow replacement surgery. Patients may need to wear protective dressings, follow strict activity restrictions, and attend close postoperative monitoring to encourage optimal wound healing. This aspect of elbow surgery requires extra care and attention from both the surgical team and the patient.
How Elbow Replacements Differ From Your Natural Joint
All joint replacements—whether hip, knee, or elbow—come with certain activity limitations. But elbow replacements tend to come with stricter long-term restrictions compared to other joint replacements.
Most elbow prostheses are made from a combination of metal and plastic. While these materials are durable, they’re not indestructible. Wear and tear on these components can eventually lead to loosening or failure of the joint replacement over time.
With hip and knee replacements, patients are generally encouraged to return to many normal activities, though high-impact sports are usually discouraged. But with elbow replacements, the guidelines are far more conservative.
Most experienced surgeons, including those at the Mayo Clinic—recognized as global leaders in elbow replacement—recommend that patients lift no more than 5 pounds with the affected arm in a single lift, or 2 pounds repetitively. This means everyday activities like carrying groceries, lifting a child, or pushing heavy objects may require modifications.
Will your elbow fall apart if you occasionally exceed those limits? Probably not. But repeated overuse or lifting beyond the recommended limits increases the risk of early wear and possible implant failure.
I recall a patient who came to me after having an elbow replacement done by another surgeon eight years earlier. His metal components were still well-fixed, but the plastic bearing had worn out completely. After asking more about his activities, he admitted he regularly lifted buckets weighing over 30 pounds on his farm—and he had already had the bearing replaced once before.
Elbow replacements simply aren’t designed for heavy, repetitive lifting. While materials and techniques may improve in the future, we’re not there yet.
When Elbow Replacements Are Used for Severe Fractures
Besides arthritis, another scenario where elbow replacement may be considered is in the treatment of complex elbow fractures. These are usually fractures of the distal humerus—the end of the upper arm bone near the elbow.
In younger patients with good bone quality, these fractures are often treated with surgical fixation using plates and screws. But in older adults, especially those with osteoporosis or severely crushed joint surfaces, internal fixation may not be possible or reliable.
In those select cases, elbow replacement may be the better option. The goal is to restore function and relieve pain when conventional fixation methods would likely fail.
However, this option is generally reserved for low-demand patients—typically older adults who do not engage in heavy physical activities. The expectation is that the replacement will last the rest of the patient’s life without requiring revision surgery. For younger, more active patients, joint-preserving options are usually preferred if feasible.
What Are the Risks of Elbow Replacement?
Every surgical procedure carries risks, and elbow replacement is no exception. Besides the wound healing risks already discussed, other potential complications include:
- Infection: The risk is slightly higher compared to other joint replacements due to the thin soft tissue coverage.
- Implant loosening: Over time, the implant may loosen from the bone, especially if weight-bearing guidelines are not followed.
- Nerve injury: The ulnar nerve, which runs near the elbow, can be stretched or compressed during surgery.
- Joint stiffness or instability: Though the replacement is designed to improve motion, some patients experience stiffness or even instability.
- Revision surgery: If the implant wears out, loosens, or causes other problems, additional surgery may be necessary.
Choosing a skilled, experienced surgeon who understands both the technical and biological challenges of elbow replacement is critical to minimizing these risks.
What Should You Expect After Surgery?
Recovery from elbow replacement varies by patient, but generally includes:
- A period of immobilization in a splint or brace
- Close wound monitoring and protection of the surgical site
- Gradual physical therapy focused on gentle motion—often avoiding strengthening for several months
- Strict adherence to weight-bearing precautions for life
Patients should have realistic expectations. The goal of elbow replacement is usually to reduce pain and restore a functional range of motion for everyday activities—not to allow return to heavy labor or sports.
Is Elbow Replacement Right for You?
Elbow replacement can be life-changing for the right patient—but it’s not for everyone. If you’re dealing with severe arthritis, a complex fracture, or debilitating elbow pain that limits your daily life, it may be worth exploring whether this procedure could help.
On the other hand, if you’re a younger, active person or someone who relies on heavy lifting for work or recreation, elbow replacement may not be the ideal solution. Other treatment options like joint-preserving surgery, injections, or activity modification might be better suited for you.
How to Find the Right Surgeon for Elbow Replacement
Because elbow replacements are far less common than knee or hip replacements, fewer surgeons are highly experienced with the procedure. If you’re considering this surgery, it’s important to seek a consultation with a fellowship-trained orthopedic specialist who focuses on elbow care.
I’ve dedicated my practice to the treatment of complex shoulder and elbow conditions, and I’m committed to giving patients honest, realistic advice about their options. Whether you’re exploring surgery or want to understand non-surgical treatments, I’m here to help guide you through your choices.
Ready to Learn More?
If you’re considering elbow replacement or want a personalized consultation, contact our office today. We serve patients throughout Western New York, northern Pennsylvania, and southern Ontario with three convenient locations in Williamsville, Orchard Park, and Niagara Falls.
Our goal is to help you make the best decision for your health—whether that means surgery or other treatment options.
