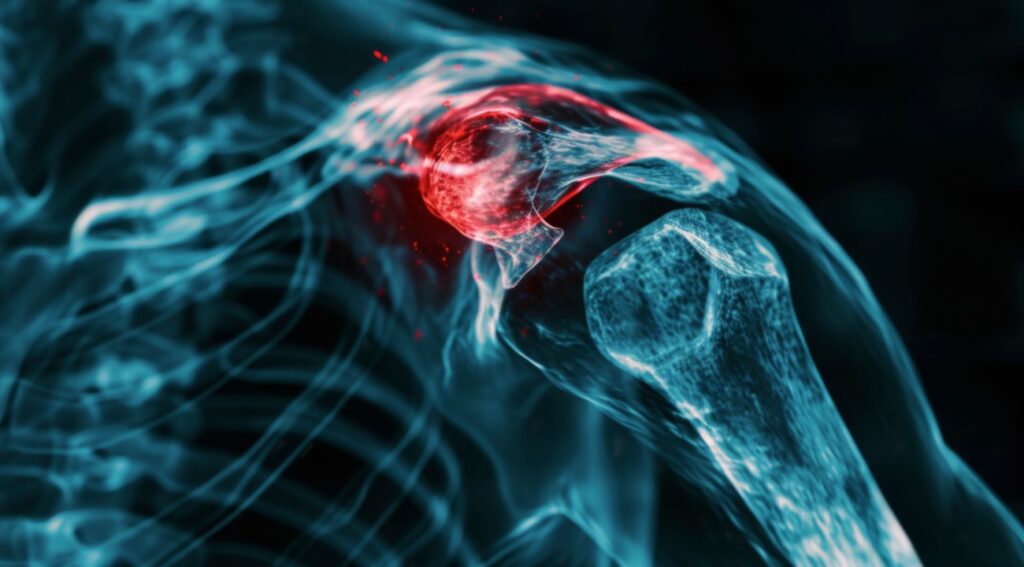
Understanding Frozen Shoulder, Rotator Cuff Tears, and Shoulder Arthritis from a Surgeon Who Treats It All
Shoulder pain affects millions of people, but no two cases are exactly alike. In this video presentation, Dr. Matthew DiPaola—an orthopedic surgeon specializing in shoulder and elbow care—explains why personalized treatment matters and walks through three common shoulder conditions that often have more than one path to relief. If you’re just beginning your search for answers or considering surgery, this talk offers valuable insights to guide your decision-making.
The Core Message: It’s All About You
Dr. DiPaola opens with a message that reshapes how we think about treatment: shoulder care isn’t one-size-fits-all. Every patient is different—different goals, different activity levels, different medical histories—and those differences play a critical role in choosing the right treatment. What works for one person might not be best for another.
Many patients try to compare their situation to a family member’s or friend’s experience. But as Dr. DiPaola explains, even if two people have the same diagnosis, the best treatment can vary significantly depending on lifestyle, pain tolerance, and long-term goals.
Three Common Shoulder Conditions – And Why They Don’t Have Just One Solution
Dr. DiPaola highlights three frequently seen conditions:
1. Adhesive Capsulitis (Frozen Shoulder)
Frozen shoulder causes stiffness, pain, and reduced range of motion due to inflammation and tightening of the joint capsule. It may come on gradually (idiopathic) or follow trauma or surgery.
Key Points:
- Risk factors include diabetes, thyroid disorders, and being female in midlife.
- Many cases resolve naturally over 9–18 months.
- Treatment can range from doing nothing to physical therapy, anti-inflammatories, and steroid injections.
- Surgery is rarely needed and only considered when conservative measures fail.
Important takeaway: A frozen shoulder can look alarming on an MRI, but the real key to diagnosis is a physical exam. Stiffness is the hallmark symptom, and treatment should be based on how you function—not just imaging results.
Learn more: How to Recover from a Frozen Shoulder >
2. Rotator Cuff Tears
The rotator cuff is made up of four muscles and their tendons that surround the shoulder joint, stabilizing it and helping with movement. Tears can range from mild fraying to full-thickness ruptures.
Key Points:
- Rotator cuff tears can be acute (from an injury) or chronic (developing over time).
- Not all tears require surgery—even some full-thickness tears can be managed non-surgically.
- Symptoms like weakness, pain, and limited range of motion vary widely.
- Treatment depends on age, tear size, activity level, and how the tear affects daily life.
Dr. DiPaola emphasizes the importance of understanding which tendon is torn, how long it’s been torn, and your goals before making a treatment decision.
Learn more: Understanding Rotator Cuff Tears >
3. Shoulder Arthritis
There are two primary joints in the shoulder that can develop arthritis: the AC joint (where the collarbone meets the shoulder blade) and the glenohumeral joint (the ball-and-socket).
Key Points:
- Glenohumeral arthritis is often driven more by genetics than wear-and-tear.
- Many people with arthritis manage well for years without surgery.
- Conservative treatments include injections and anti-inflammatory medication.
- Shoulder replacement is an effective option—but only when symptoms are severe and other treatments have failed.
Dr. DiPaola reminds us that the right time for shoulder replacement depends on your lifestyle and tolerance for discomfort. For one active patient in his 70s, injections were enough. Another, with similar imaging and age, opted for surgery.
Learn more: Shoulder Arthritis: What Are Your Options? >
Making the Right Choice: The Conversation Matters
There is rarely one single “correct” treatment for shoulder pain. That’s why Dr. DiPaola stresses the importance of shared decision-making between patient and physician. His role is to help clarify options, explain risks and benefits, and guide patients toward the path that fits them best.
Treatment choices depend on factors like:
- Age and activity level
- General health and medical history
- Type and severity of the condition
- Personal priorities, pain tolerance, and lifestyle goals
Dr. DiPaola’s approach isn’t just about fixing a shoulder—it’s about treating the whole person.
Don’t Let Imaging Define Your Treatment
One of the most important lessons from this talk is that MRI results don’t always tell the whole story. Many people have tears or arthritis that show up on imaging but aren’t the source of their pain. That’s why physical examination and patient history are essential.
If you’re facing shoulder pain, the next step isn’t always surgery. In fact, the right answer might be to do less—not more. The key is having the right guide.
Watch Dr. DiPaola’s full presentation above for a deeper understanding of how shoulder conditions are diagnosed and treated—and why individualized care matters more than ever.
